Bristol photographer Tom Skipp has been working with the UNCOVER Group to understand the human stories and motivations behind the people who are playing a role in global efforts to overcome COVID-19.
Tom was concerned by what he felt was a public distrust of science and an anecdotal feeling that minority populations might be dissuaded to take a vaccine given a historic prejudice by institutions. He felt that scientists are perceived as inaccessible, usually only seen on pedestals or next to government officials disseminating statistics, and limiting civil liberties.
 By meeting some of the people involved in the UNCOVER group, Tom hoped to understand their stories and motivations and relate those to the people of Bristol on a street level. Tom has captured a series of portraits some of which are part of a billboard campaign on show at various locations across Bristol until the 9th May.
By meeting some of the people involved in the UNCOVER group, Tom hoped to understand their stories and motivations and relate those to the people of Bristol on a street level. Tom has captured a series of portraits some of which are part of a billboard campaign on show at various locations across Bristol until the 9th May.
Dr Rajeka Lazarus, consultant in infectious diseases and microbiology at University Hospitals Bristol and Weston, runs COVID vaccine trials and has been motivated by the impact of COVID on minoritized populations.
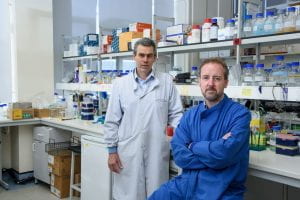
Dr Ore Francis, a post-doctoral research assistant developing a SARS-CoV-2 pseudovirus to make COVID research faster and safer. He has been motivated by the generosity of people donating samples and resourced to the global COVID research efforts.
Talking about his project, Tom said: “These photographs are all taken where the people have been carrying out their work over the last year, in university labs, hospitals and at home. They’ve all been experiencing the daily struggles and burdens put upon all of us by the pandemic with the added pressure of having the capabilities to do something about it.”
- 92-98 Kingsland Road, BS2 0QZ – Drs Ore Francis, Research Associate, and Rajeka Lazarus, a consultant in infectious diseases and microbiology at UHBW
- 28 Stapleton Road, BS5 0QX – Dek Woolfson, Professor of Chemistry and Biochemistry and Director of the Bristol BioDesign Institute
- 34 Ashley Road, BS6 5NS – Adam Finn, Professor of Paediatrics at Bristol, Director of the Bristol Vaccine Centre at Bristol Medical School and lead of Bristol UNCOVER Group
- 265 Church Road, BS5 9HU – Dr David Mathews, Reader in Virology
- Electric Ladyland, Trinity Road, BS2 0FJ – Dr Christy Waterfall, Senior Research Associate
Image credit: Tom Skipp